Introduction
In digital medical imaging, the way images are presented on the screen can be just as important as the quality of the images themselves. Radiologists often deal with hundreds of slices or multiple views per patient, and manually arranging them wastes valuable time. This is where the concept of a hanging protocol becomes essential.
A hanging protocol defines the rules by which images are automatically displayed in a DICOM viewer. Instead of dragging, resizing, and organizing images for every case, the system arranges them consistently and intelligently according to predefined standards. For mammography and tomosynthesis—modalities with high data volume and multi-view requirements—hanging protocols are especially critical.
What is a Hanging Protocol?
In simple terms, a hanging protocol is a recipe for how to display images on a workstation. It includes rules like:
-
Which images go into which monitor or viewport
-
How to order current and prior exams
-
Zoom, window/level, and orientation defaults
-
Synchronization of scrolling across views
By following a hanging protocol, a viewer ensures that every time a radiologist opens a study, the images appear in a familiar, predictable way—ready for diagnostic interpretation.
Why Hanging Protocols Matter in Mammography
Mammography is unique because each exam typically contains multiple standard views of each breast: CC (craniocaudal), MLO (mediolateral oblique), and sometimes additional spot views. Radiologists need to see them side by side, often comparing left and right breasts, as well as current and prior exams.
Without hanging protocols, organizing these images manually can be tedious and prone to error. With them, the system automatically places:
-
Left CC next to Right CC
-
Left MLO next to Right MLO
-
Prior mammograms beneath or adjacent to the current ones
This structure supports rapid, accurate side-by-side comparison, which is essential for detecting subtle asymmetries, microcalcifications, or interval changes that could indicate early breast cancer.
Hanging Protocols for Tomosynthesis (DBT)
Digital Breast Tomosynthesis (DBT) adds another layer of complexity. Each breast may generate hundreds of slices instead of just two or four images. Radiologists must scroll through these slices while also keeping the standard 2D views in context.
A hanging protocol for tomosynthesis typically includes:
-
Displaying DBT slices in a large primary viewport
-
Keeping synthetic 2D images visible in a secondary viewport
-
Synchronizing slice scrolling with reference markers
-
Linking prior DBT studies for parallel scrolling and comparison
This structured layout reduces cognitive load and ensures that radiologists don’t miss important findings hidden within the slice stack.
Compare and Prior Exams within Hanging Protocols
An effective hanging protocol doesn’t just arrange the current exam—it also manages prior exams. For mammography, prior images are crucial to identify whether a finding is new, stable, or changing. A good hanging protocol will:
-
Automatically retrieve priors for the same modality
-
Place them in the same layout as current images
-
Synchronize scrolling and zoom across current/prior pairs
This integration makes it much easier to track subtle changes across years of exams, which is essential in breast imaging.
Benefits of Hanging Protocols
-
Consistency – Every exam is displayed in the same way, reducing variability.
-
Efficiency – Radiologists save time by avoiding manual arrangement.
-
Accuracy – Side-by-side placement of standard views improves diagnostic confidence.
-
Workflow integration – Protocols align with modality-specific needs (e.g., tomosynthesis slice navigation).
-
Scalability – Large volumes of data can be managed systematically.
Challenges and Customization
While hanging protocols are powerful, they are not one-size-fits-all. Radiologists may prefer different layouts depending on their subspecialty or even personal habit. Some challenges include:
-
Handling unusual or additional views (spot compression, magnification)
-
Managing different display monitor setups (1, 2, or 4 monitors)
-
Integrating priors from different vendors or with slightly different metadata
Therefore, modern systems allow customizable hanging protocols that can be saved per user, per modality, or per department.
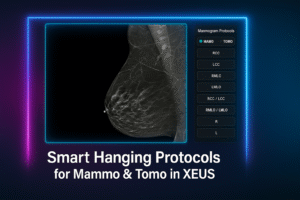
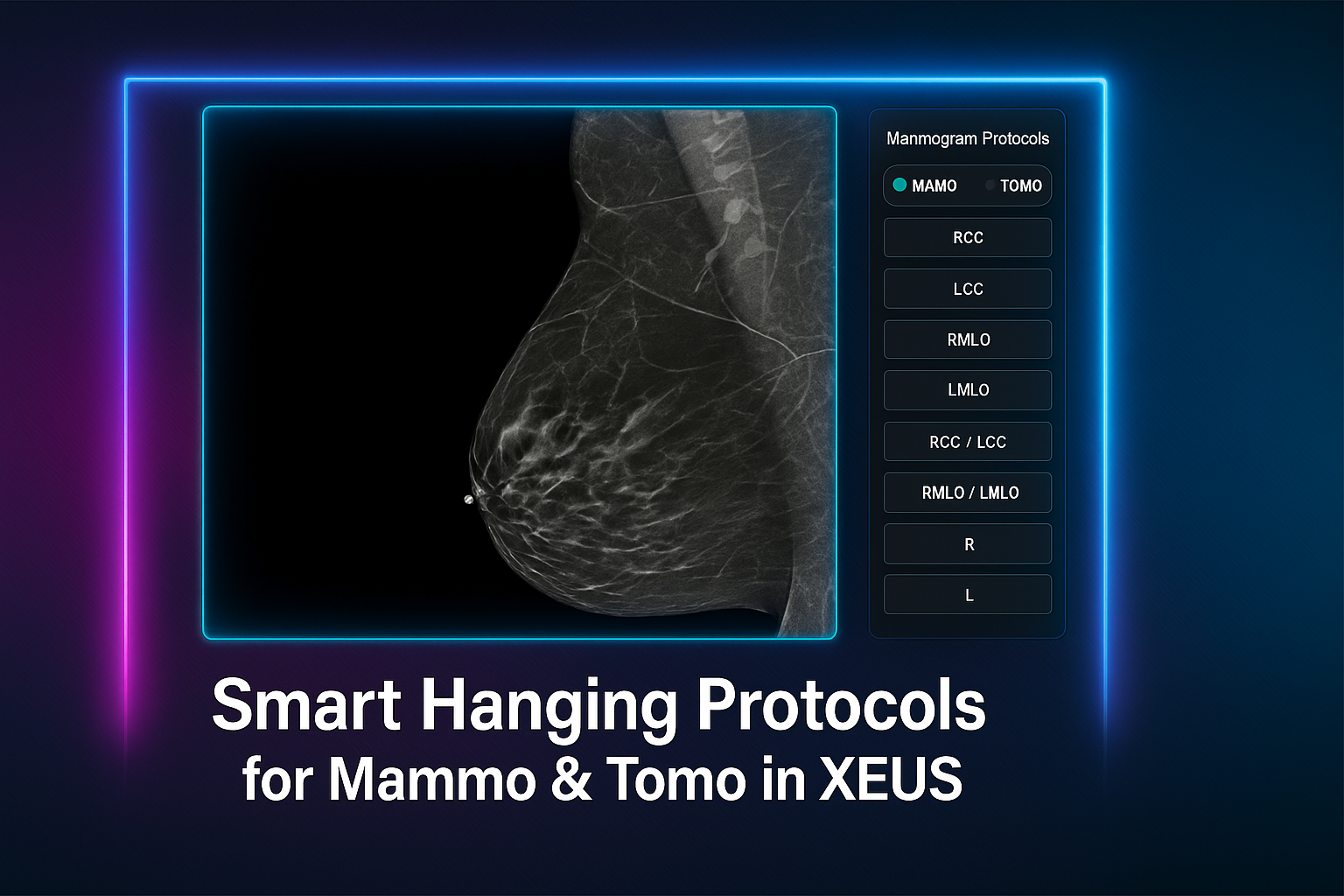
Smart Hanging Protocols for Mammo & Tomo in XEUS
Reading mammography and tomosynthesis shouldn’t be slowed down by complex setup. That’s why XEUS introduces specialized hanging protocols designed specifically for breast imaging.
With XEUS, the most commonly used hanging layouts are already built in as one-click buttons. Radiologists can simply switch between them instantly, moving from CC/MLO views to DBT slice stacks or synthetic 2D images with zero hassle.
This means:
-
Speed: No more manual arranging—your preferred layouts are always one button away.
-
Specialization: Protocols optimized for mammography and tomosynthesis, reflecting real clinical needs.
-
Flexibility: Easy toggling between different hanging presets during a single reading session.
The result? Radiologists get exactly the views they need, exactly when they need them—streamlined, intuitive, and consistent.
XEUS makes advanced breast imaging not only accurate, but effortless.
Conclusion
Hanging protocols are the silent backbone of efficient medical imaging workflows. For mammography and tomosynthesis, where comparison and multi-view analysis are central, they are indispensable. By automatically arranging images in logical, modality-specific layouts, hanging protocols save time, improve accuracy, and reduce the risk of oversight.
With XEUS by MiNNOVAA, radiologists gain an intelligent, user-friendly solution that makes hanging protocols work seamlessly—especially for the complexities of breast imaging.
Hanging protocol in XEUS: faster, smarter, and built for precision.
for more information: https://academy.minnovaa.com/mod/page/view.php?id=38
References:
- DICOM PS3.17 – Explanatory Information (Hanging Protocol IOD example
🔗 https://dicom.nema.org/medical/dicom/current/output/chtml/part17/PS3.17.html -
DICOM PS3.16 – Hanging Protocol Context Groups
🔗 https://dicom.nema.org/medical/dicom/current/output/chtml/part16/chapter_B.html -
ACR Digital Mammography QC Manual – Image Display and Comparison
🔗 https://www.acr.org/Clinical-Resources/Quality-and-Safety/Resources/Digital-Mammography-QC -
Radiology Society of North America (RSNA): Tomosynthesis in Breast Imaging
🔗 https://pubs.rsna.org/doi/full/10.1148/radiol.2016151789 -
Society for Imaging Informatics in Medicine (SIIM): Best Practices in Hanging Protocols and Display Consistency
🔗 https://siim.org/page/enterpriseimaging